Fertility Screening: A Step-by-Step Guide
- doctor4701
- Oct 9, 2025
- 5 min read
A fertility screening can detect common reproductive problems early—while there is still time to act. Early answers give couples clarity on whether lifestyle adjustments, medications, or assisted reproductive techniques such as IUI or IVF offer the best path toward starting a family.
This guide explains who should get tested, what each fertility check involves, and how results shape your next steps in Singapore.
Why Consider Fertility Screening?
Fertility screening is valuable for any couple planning pregnancy, not just those already struggling with infertility. It offers a clear picture of reproductive health before precious time is lost.
Benefits of fertility screening:
Early identification of fertility issues – Detects potential problems like irregular ovulation, poor ovarian reserve, or abnormal sperm quality, enabling timely intervention.
Detection of underlying health conditions – Tests can reveal endometriosis, fibroids, premature ovarian insufficiency, PCOS, or thyroid disease, which affect fertility and overall health.
Reduced emotional and financial stress – Knowing the cause early prevents years of uncertainty and allows couples to plan and budget for future treatment.
Greater control over family planning – Results guide whether to pursue lifestyle optimisation, fertility preservation, or assisted reproduction such as IUI or IVF.
When should you consider fertility testing?
You’re under 35 and have tried to conceive for 12 months without success.
You’re 35 or older and have tried for 6 months without success.
You have irregular or absent periods, past STIs, chemotherapy, or pelvic surgery.
You or your partner has a known reproductive issue (e.g., blocked fallopian tubes, low sperm count).
Preparing for Your Appointment
Your fertility specialist needs a complete health picture to interpret your results. Be ready to provide the following information:
Pregnancy history – Previous pregnancies, miscarriages, or complications.
Medical conditions – Diabetes, thyroid disease, PCOS, or endometriosis.
Lifestyle details – Diet, exercise, alcohol, smoking or vaping.
Family history – Infertility, early menopause, genetic conditions.
Medications and supplements – As some can interfere with ovulation or implantation.
Typical fertility tests include:
Hormonal blood tests – FSH, LH, oestradiol (ovulation), testosterone (if PCOS suspected).
AMH (Anti-Müllerian Hormone) – Estimates ovarian reserve and potential egg supply.
Thyroid function test – Checks TSH and related hormones, as thyroid imbalance disrupts ovulation.
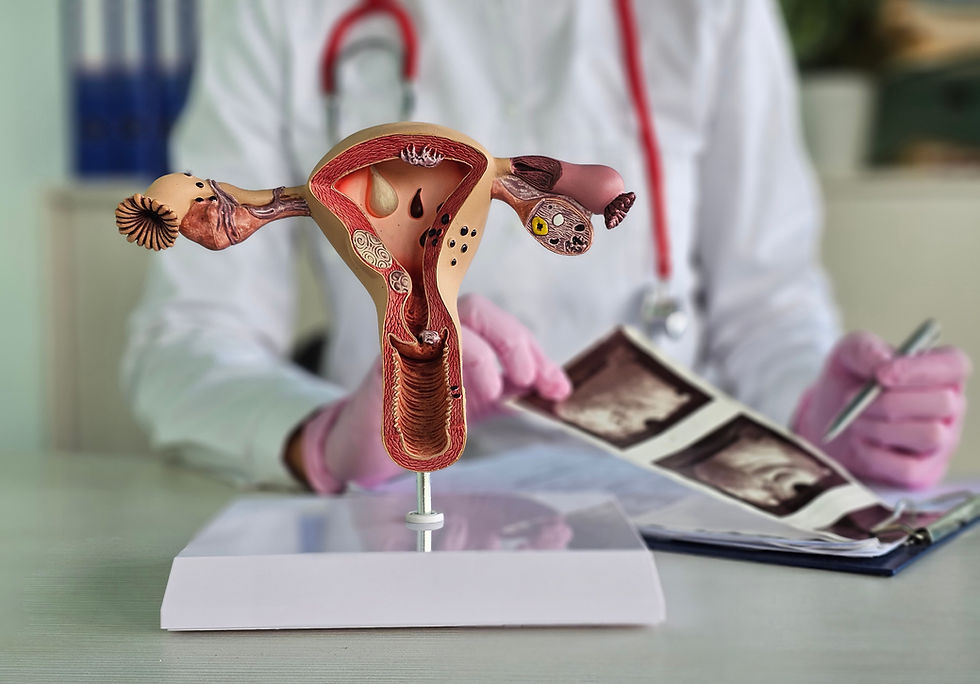
Ultrasound imaging – Counts resting follicles, checks womb structure and lining, detects fibroids or ovarian cysts.
Hysterosalpingogram (HSG) – X-ray with dye to confirm if fallopian tubes are patent.
Genetic screening – Recommended if there’s family history of inherited disorders or recurrent miscarriage.
General health checks – BMI, blood pressure, metabolic risk markers.
Semen analysis – Assesses sperm count, motility, and morphology.
Advanced sperm function tests – DNA fragmentation or oxidative stress testing when standard semen analysis is borderline.
When should you consider fertility testing?
You’re under 35 and have tried to conceive for 12 months without success.
You’re 35 or older and have tried for 6 months without success.
You have irregular or absent periods, past STIs, chemotherapy, or pelvic surgery.
You or your partner has a known reproductive issue (e.g., blocked fallopian tubes, low sperm count).
Preparing for Your Appointment
Your fertility specialist needs a complete health picture to interpret your results. Be ready to provide the following information:
Pregnancy history – Previous pregnancies, miscarriages, or complications.
Medical conditions – Diabetes, thyroid disease, PCOS, or endometriosis.
Lifestyle details – Diet, exercise, alcohol, smoking or vaping.
Family history – Infertility, early menopause, genetic conditions.
Medications and supplements – As some can interfere with ovulation or implantation.
Typical fertility tests include:
Hormonal blood tests – FSH, LH, oestradiol (ovulation), testosterone (if PCOS suspected).
AMH (Anti-Müllerian Hormone) – Estimates ovarian reserve and potential egg supply.
Thyroid function test – Checks TSH and related hormones, as thyroid imbalance disrupts ovulation.
Ultrasound imaging – Counts resting follicles, checks womb structure and lining, detects fibroids or ovarian cysts.
Hysterosalpingogram (HSG) – X-ray with dye to confirm if fallopian tubes are patent.
Genetic screening – Recommended if there’s family history of inherited disorders or recurrent miscarriage.
General health checks – BMI, blood pressure, metabolic risk markers.
Semen analysis – Assesses sperm count, motility, and morphology.
Advanced sperm function tests – DNA fragmentation or oxidative stress testing when standard semen analysis is borderline.
Interpreting Your Results
Once your results are in, your doctor explains how the numbers and images affect your fertility outlook.

Ovarian-reserve markers
AMH: Indicates egg pool size. Low AMH means reduced egg supply.
FSH: High levels suggest the ovaries need more stimulation, indicating declining egg reserve.
Antral Follicle Count (AFC): More follicles = higher ovarian reserve, guiding IVF medication dosing.

Structural findings
Pelvic ultrasound: Detects abnormal uterine structure, fibroids, ovarian cysts, or polycystic ovary morphology.
HSG/Sono-HSG: Determines if fallopian tubes are patent. One open tube still allows natural conception.
Male fertility indicators
Semen analysis: Confirms whether sperm count, shape, or motility is contributing to infertility.
Next Steps After Screening
Your fertility plan depends on test outcomes. Some may need only minor lifestyle changes; others require medical or assisted-reproduction interventions.
Lifestyle Optimisation
Balanced diet: Low glycaemic foods, lean protein, vegetables, whole grains.
Regular exercise: 150 minutes of moderate activity weekly improves insulin and hormone balance.
Supplements: Folic acid, vitamins B6, B12, and vitamin D for egg and sperm health.
Medical Management
Thyroid treatment: Medications to normalise under- or overactive thyroid function.
Insulin regulation: Metformin or Inositol for PCOS to improve ovulation.
Hormone rebalancing: Short courses of contraceptives, progesterone, or anti-androgens to regulate cycles.
Assisted-reproduction options
Ovulation induction: Clomiphene citrate, letrozole, and/or low-dose gonadotropins stimulate egg release.
IUI (Intrauterine Insemination): Processed sperm placed directly into the uterus to overcome mild male or unexplained infertility.
IVF (In-Vitro Fertilisation): Eggs are fertilised outside the body and best embryos are transferred to the uterus. Ideal for blocked tubes, severe male-factor, or repeated IUI failure.
ICSI (Intracytoplasmic Sperm Injection): A single sperm injected into an egg, used when sperm quality is very low.
When to re-test or escalate care
Every 6–12 months: Repeat AMH, FSH, or AFC if delaying pregnancy.
After 3 failed ovulation-induction cycles: Consider IUI or IVF.
Immediately: Seek review if new symptoms (pelvic pain, abnormal bleeding, sudden weight gain) appear.
Fertility Screening at Daniel Koh Clinic for Women and Fertility Services
At Daniel Koh Clinic, our fertility screening program is comprehensive, personalised, and evidence-based. From initial blood tests and ultrasound to advanced genetic and sperm testing, Dr Daniel Koh tailors investigations and treatments to your age, reproductive goals, and medical background.
His dual expertise in reproductive medicine and maternal–fetal medicine ensures seamless care, from the first consultation and fertility treatments such as IUI or IVF, through pregnancy monitoring, right up to delivery.
📞 Contact Daniel Koh Clinic today to schedule your fertility screening and take the next step toward starting your family.
.png)




Comments